Arteriovenous Malformation (AVM)
Normally, blood flows from the heart to the arteries of the body. The arteries branch and get smaller until they become a capillary, which is just a single cell thick. In this way blood pressure drops to very low levels that the thinner walled veins can cope with. In an AVM, usually early in life, arteries connect directly to veins. This is a high-pressure shunt or fistula. Veins are not able to handle the pressure of the blood coming directly from the arteries. The veins stretch and enlarge and create what we call a ‘nidus’. Usually, there are multiple feeding vessels in an AVM and many draining veins.
How can an AVM be treated?
Endovascular techniques are now the main route of treatment for AVMs. This involves treating the AVM through the blood vessel system.
Through a pinhole incision, a catheter is placed into an artery in the groin area and passed to the AVM using x-ray guidance. Once in the correct vessel, an embolic material such as a coil or glue is placed into the abnormal communication cutting off the blood supply, in turn shrinking and shutting down the AVM. This procedure requires no stitches, downtown or major incision and can be done under moderate IV sedation.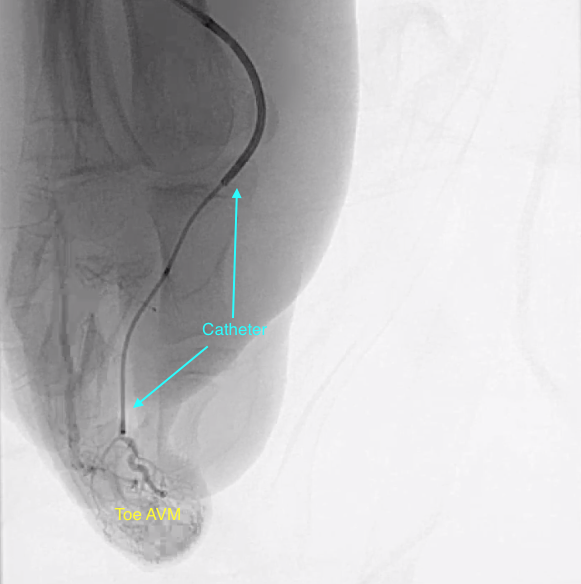
Venous Malformation
A venous malformation is a congenital defect of the veins. The veins are different than normal veins and contain, for example, less muscle cells. Feeding them less blood, which is actually their duty. That is why they sometimes look varicose. A venous malformation can be anywhere in the skin or in the body. Usually it is a venous malformation blue. A venous malformation feels soft and sometimes it can be empty. It is unclear why a venous malformation occurs exactly. Usually this gives cosmetic problems, sometimes pain. However, there may also be functional problems, as with a large deviation on the lip.
Important is the difference with the infantile hemangioma. Venous malformations are defects of the veins and exist from birth. Venous malformations grow along with the child and do not go away by themself (hemangiomas occur almost always after birth, then grow very fast; they can be quite large and then will go away).
Usually, the diagnosis may be made on the based on the history and look at the area. If the doctor is not sure he can order an ultrasound or a CT scan.
If treatment is required, it is typically treated with sclerotherapy. It is something sprayed in the blood vessels by an Interventional Radiologist that provides a chemical reaction which makes the walls of the blood vessels there decrease. This makes the place invisible. Correction is also possible with surgery or laser treatment. A deviation that is in the legs can also be treated with support stockings.
What is a lymphatic malformation?
A lymphatic malformation is an abnormality of the lymphatic system. The lymphatic system forms part of the immune system that identifies and fights off invaders, such as bacteria and viruses consisting of a network of vessels within the body through which lymph circulates, and many lymph nodes which filter the lymph fluid and help the body fight infection. The specific symptoms and severity of lymphatic malformations varies based upon the size and specific location of the malformation. Some lymphatic malformations can be massive. Lymphatic malformations regardless of size can potentially cause functional impairment of nearby structures or organs and disfigurement of affected areas.
How can lymphatic malformations be treated?
There are two main options for treatment: sclerotherapy and surgical removal.
Sclerotherapy
This is a procedure carried out by an interventional radiologist, who shrinks the lymphatic vessels by injecting a special substance through the skin under general anaesthetic. It may require several sclerotherapy sessions and even then, it might grow again.
Surgical removal
Sometimes, lymphatic malformations can be removed safely. Detailed scans will be needed to plan the operation. There will be a certain amount of scarring after the operation, as with all surgery.
The above information is not all inclusive of the risks, alternatives and benefits. It is not meant to be a substitute for informed discussion between you and your doctor, but can act as a starting point for such a discussion. There are complications possible with any medical procedure. Overall, minimally invasive procedures have a lower complication rate than open surgeries.




