Mesenteric Ischemia
Mesenteric ischemia occurs when one or more of your mesenteric arteries become obstructed. As a result of the obstruction, your intestines do not receive an adequate amount of oxygen, and therefore cannot function properly. Over time, tissue in your intestines can die due to inadequate blood flow. Mesenteric ischemia usually affects your small intestine, but can also impact other organs such as your stomach, colon or liver.
It can come on suddenly, known as acute mesenteric ischemia, or gradually, known as chronic mesenteric ischemia. Acute disease often presents with sudden severe pain. Symptoms may come on more slowly in those with acute on chronic disease. Signs and symptoms of chronic disease include abdominal pain after eating, unintentional weight loss, vomiting, and being afraid of eating.
Risk factors
Atrial fibrillation, heart failure, chronic renal failure, being prone to forming blood clots, and previous myocardial infarction.
Mechanism
Acute mesenteric ischemia often occurs when a blood clot (embolus), which usually forms in the heart, travels into one of the mesenteric arteries and blocks the blood flow. People with an irregular heartbeat are at a higher risk for acute mesenteric ischemia.
Chronic mesenteric ischemia is commonly caused by atherosclerosis (hardening of the arteries). This occurs when a sticky substance, called plaque, builds up in your arteries and causes them to narrow and stiffen.
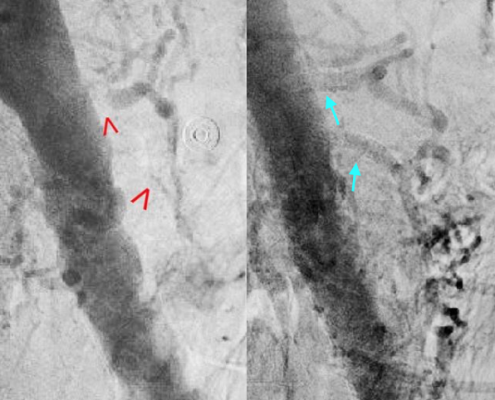
There are four mechanisms by which poor blood flow occurs: a blood clot from elsewhere getting lodged in an artery, a new blood clot forming in an artery, a blood clot forming in the mesenteric vein, and insufficient blood flow due to low blood pressure or spasms of arteries. Chronic disease is a risk factor for acute disease. The best method of diagnosis is angiography, with computer tomography (CT) being used when that is not available.
Treatment
Treatment of acute ischemia may include stenting or medications to break down the clot provided at the site of obstruction by interventional radiology. Open surgery may also be used to remove or bypass the obstruction and may be required to remove any intestines that may have died. If not rapidly treated outcomes are often poor. Among those affected even with treatment the risk of death is 70% to 90%. In those with chronic disease bypass surgery is the treatment of choice. Those who have thrombosis of the vein may be treated with anticoagulation such as heparin and warfarin, with surgery used if they do not improve.
The above information is not all inclusive of the risks, alternatives and benefits. It is not meant to be a substitute for informed discussion between you and your doctor, but can act as a starting point for such a discussion. There are complications possible with any medical procedure. Overall, minimally invasive procedures have a lower complication rate than open surgeries.